Needlessly Slow & Complex Patient Enrollment Brings Costly Delays & Risks
New patients need to fulfill several steps before they join a healthcare provider and visit a doctor, nurse or other healthcare practitioner.
But as healthcare providers know all-too-well, enrolling new patients is often a hugely data-intensive process for everyone involved - from the patient, their previous doctor or healthcare provider, payer or a third-party administrator (TPA), and their employer group.
To be registered as a patient, a customer is typically asked to complete a slew of forms, and provide multiple IDs, supporting documents and consents, including:
- Completing intake forms, a health risk assessment (HRA) or other medical questionnaires
- Provide payer information such as their health insurer, TPA, or employer group
- Verify ID - requiring their social security number (SSN) and driver’s license, and in some cases even a birth certificate or green card
- Transfer previous medical records from their most recent provider
- Give legally binding consent to a Notice of Privacy Practices, which authorizes providers to use and share their protected health information (PHI) under the HIPAA privacy rule.
- Provide additional supporting medical, financial, and legal documents, such as their current prescribed medications, and in some cases proof of income, or Power of Attorney (POA) rights.
- Setting up secured and ACH electronic payments for out-of-pocket medical expenses
How is this enrollment process actually experienced by the customer?
Current patient onboarding processes to collect all of this data suffer from siloed digital systems and outdated manual processes that bounce patients between touchpoints such as face-to-face, sites or portals, the contact center and email.
For example, a customer may first call the contact center to request to join a healthcare provider. But then they’re usually asked to check their email and download crowded PDF-based forms and questionnaires that are cumbersome to fill out digitally, especially on the device customers use most - their smartphone.
Many customers delay completing these processes digitally and end up printing off all the forms and documents they need to complete. Then, they’re forced to expend more time and energy scanning or faxing all documents back to the healthcare provider. This creates several critical problems:
Prolonged wait times result in slow turnaround time
Choppy and broken processes frustrate patients that need to print, scan or fax back paper documents. But that problem is heaped right back onto healthcare staff who must sift through multiple emails and paper documents, delaying enrollment turnaround times.
Administrative overhead and rework
Retrieving and storing a wide array of patient forms and documents adds a significant burden to staff who often obtain missing information from the patient and rekey it into multiple systems. This wastes an inordinate amount of time and resources on admin tasks and paperwork, draining productivity.
Not having a comprehensive digital enrollment process is especially problematic for Medicare providers, who only have a 3-month window to complete large volumes of sign-ups.
Administrative burden and staffing resources are often exhausted, adding significant expenses needed to hire additional staff.
Flooded Call Centers
Confused and inconvenienced customers will dial the contact center repeatedly to clear up questions on forms and documents they can’t clearly understand on their own. This prolongs the onboarding process further and leads to greatly increased call volumes and burden on agents, who must field menial queries.
Inaccurate patient data due to manual errors
Time and resource-intensive manual processes lead to inevitable errors such as entering the wrong plan effective date or dependent name, which can cause significant friction with customers and lead to escalation and healthcare board complaints.
Data privacy and compliance risks
PII, PHI and medical data are extremely valuable commodities on the dark web and are leveraged by hackers for extortion and ransomware, with each stolen record selling for as much as $1,000. Emailing (or still in many cases today snail mailing) back forms and documents containing PII and PHI data opens patients and providers alike to these security risks. Providers suffering a breach may be found liable for violating HIPAA rules and be ordered to pay more than $1.7 million in penalties along with other corrective actions.
Patient Care & Servicing Processes Are Riddled with Pain & Friction for Customers & Staff
Complexities for healthcare providers only swell further when looking at the wide variety of ongoing patient needs that must be managed, including intake of existing members. Most legacy systems currently being used by providers are limited to basic appointment scheduling and payment billing and are not built to support the variety of medical, financial and legal data that come into play for many customer-facing processes.
To cover all patient needs, providers today are stitching together a patchwork of siloed digital systems to collect IDs, signatures, forms, and consents. Lack of seamless integration between them creates long, multi-step processes for seemingly simple servicing requests. And because many of these technologies still rely on legacy processes such as PDF documents and email, they make it impossible for customers to fulfill all requirements digitally - needlessly infusing paper and administrative work for staff, which compromises data accuracy and leads to non-compliance risks.
COVID-19 has exacerbated these gaps, complicating and oftentimes severely limiting in-person appointments. Not having a unified digital intake process for existing patients can detrimentally affect both patient health and experience.
Digital silos and legacy processes add this burden and complexity in nearly every instance a patient needs to change or update their medical or payer information, grant consent, or submit documents to support a request, such as:
- Change of address or medical insurance payer
- Updating insurance dependents
- Updating medical records
- Consent for medical procedures
- Consent to updated HIPAA requirements
- Releasing medical records
- Submitting receipts for a Health Savings Account (HSA), Health Risk Assessment (HRA), Transportation Security Administration (TSA), or Transportation Reimbursement Account (TRA)
- Assuming Power of Attorney (POA) rights for another patient
- Letter of medical necessity (LMN) - often needed if a patient is submitting a request or claim that was previously denied
Fragmented point solutions hurt patient care & drive up costs
Not having a unified digital process that can quickly turn around these patient needs brings friction, delay and frustration to patients who are often going through trying times and already overwhelmed with their own pain and anxiety. This can detrimentally affect both patient health and experience.
For example, a patient that’s been injured in an accident is looking to their healthcare provider to complete the intake process as quickly as possible so they can move forward with treatment and get on a care plan towards recovery.
Many providers today still typically email multiple forms to the patient, many of which are busy and confusing for patients to complete on their own, increasing the likelihood that forms will be sent with errors or important information still missing. The provider must then ask for forms or incomplete documents to be re-submitted - resulting in long, tedious, and stressful experiences for both patients and healthcare staff.
Outdated and broken patient care and servicing experiences:
- Add multiple touchpoints that fuel friction between customers and care staff
- Cause wait times and delays in delivering patient care
- Overburden back-office and customer-facing staff
- Inflate data and operational costs
- Result in errors on both sides that can cause misdiagnosis or violate compliance
Incomplete Engagement Tools Fail Both Health & Business Outcomes
Engaging and motivating patients to be more proactive in adhering to treatments, preventions and services that can improve their health and well-being is vital to providers to improve healthcare outcomes and greatly reduce strain and costs on the system through successful prevention. In fact, engaged patients have proven to be 3 times less likely to develop unmet medical issues, and twice as likely to seek care in a timely manner when compared to unengaged patients.
There are many important ways healthcare providers can engage their patients to enhance both health and business outcomes, including:
- Digital appointment scheduling
- Appointment and procedure prep instructions
- Automated patient check-in
- Condition-specific education and remote monitoring
- Providing follow-up information such as digital summaries after appointments
- Satisfaction surveys
Siloed engagement tools miss the mark with patients
The complexity of the healthcare system, cultural issues, health literacy issues, and haphazard tools that fail to engage customers on the channels most convenient for them were already major issues providers have been contending with before the COVID-19. But they have taken on unprecedented importance in light of the rapid spread of transmissions, and the massive burdens and costs the pandemic is placing on providers and staff.
Many providers today have invested in numerous methods to optimize patient engagement, including portals, mobile apps, telephony and chat software to enable appointment scheduling, send out reminders, educate on how to prepare for upcoming procedures, and conduct satisfaction surveys. But these disparate patient engagement tools are siloed and delivered across separate channels - which results in inconsistent customer experience and the annoying inconvenience of being engaged via multiple channels.
These fragmented engagement methods fail to catch up with the needs and behavior of today’s consumers who have become used to mobile experiences that are visual, intuitive, instant and seamless. 57% of Americans spend 5 hours or more on their mobile phone every day, while for 19% of millennials smartphones are the only way they connect online.
Mobile apps have not yielded the engagement providers have hoped for, as many patients are put off by the need to download a healthcare providers’ app from the store and log in each and every time they receive a notification.
Sub-par patient engagement tools undermine providers’ ability to provide important education materials to patients. A national survey by the Center for Advancing Health revealed that almost 30% lacked the basic facts and understanding of treatment requirements.
To increase engagement that meaningfully impacts both health and business outcomes, a patient engagement solution needs to:
- Integrate all capabilities for patient engagement, bidirectional communication, and compliant exchange of information with one unified platform delivering consistent customer experience.
- Enable patients to easily and quickly interact in a visual and mobile-friendly interface without needing to download an app
- Give healthcare providers real-time visibility into patient engagement activity and progress
- Instantly capture all data provided by the customer by integrating seamlessly with your EHR and all relevant backend and customer-facing systems
- Ensure end-to-end encryption to protect patient data and ensure HIPAA compliance
Streamlining Digital Experience & Engagement Throughout the Patient Lifecycle
Customers that have already experienced painfully bureaucratic and inconvenient experiences every time they turned to their healthcare provider are far less engaged down the line.
For healthcare systems, medicare providers and DSOs, successful patient engagement must span the entire patient lifecycle, beginning with enrollment, supporting quick, efficient and compliant access to care, and proactively engaging them on the channels most convenient for them with the knowledge they need to be more active in their own care.
This requires reimagining current patient interactions and eliminating the digital silos and outdated legacy processes that frustrate customers with long and complicated onboarding, care delivery and coverage, overwhelm healthcare employees, and harm compliance.
It’s time for a smarter and digitally complete approach to patient engagement.
To put an end to broken patient experiences, siloed digital systems and paperwork need to make way for one unified compliant platform that digitizes all patient interactions from start to finish.
By leveraging Digital Completion technology to digitize patient onboarding, servicing, and engagement end-to-end, providers can capture all requirements they need from patients in one secure and compliant digital session optimized for mobile.
Instead of requiring customers to download multiple legacy PDF forms and bouncing them across online and offline channels, healthcare patients today can simply open an SMS or email link from wherever they are on their smartphone, where they can simply tap and swipe through each step they need to complete in one intuitive, real-time interactive digital session, including eSignatures, ID verification, document collection, and digital consent of terms and conditions.
Providers can build intelligent and automated workflows based on conditional logic, that ensure patients only see and complete the actions needed - no more, no less. This enables employees to complete the process faster, with fewer errors, and greater clarity about any next steps.
For healthcare providers, accelerating processes all in one digital platform enables them to reduce significant staffing and overhead costs demanded by paper-heavy admin tasks, freeing up employees to focus on delivering the best care possible to patients.
Having one end-to-end secure digital audit trail minimizes confusion and errors on both sides, accelerating care processes and ensuring 100% compliance.
The huge opportunity of completely digital patient engagement
Completing healthcare processes and engagement digitally and compliantly allows healthcare providers to:
1) Improve patient experiences across the board:- Enroll new patients quickly and efficiently directly from their smartphone, accelerating acquisition for healthcare systems, medicare providers, and DSOs.
- Eliminate misunderstandings and errors from patients and staff by verifying ID and collecting all required signatures, documents, consents and payments securely and compliantly in one digital platform
- Enable patients to easily and quickly complete requests, update personal information, medications, dependents, and payer information from their mobile phone
2) Lower operational costs and overhead:
- Cut time and resources wasted on manual processes and paper-heavy admin work for both clinical and non-clinical staff
- Reduce call center volume and alleviate workload burdens, reduce staffing overhead caused by inefficient time-consuming processes
- Reduce burnout and related turnover costs by enabling better productivity by eliminating the drain of avoidable administrative tasks, allowing staff to focus more time on one-to-one patient care
3) Reduce revenue leakage:
- Improves closure rates for referrals
- Reduces no-shows and misunderstandings that result in poor or wrong prep for procedures (e.g. colonoscopies)
- Improves treatment and increases preventive care by patients, adding up to increased revenue and profitability for healthcare providers
4) Enhance patient engagement and satisfaction:
- Increase satisfaction by communicating with patients at the right time and on the channel they engage with most
- Produce greater engagement by deploying regular, personalized, conversational messages that motivate patients to act
Healthcare providers delivering digitally complete patient experiences are achieving:
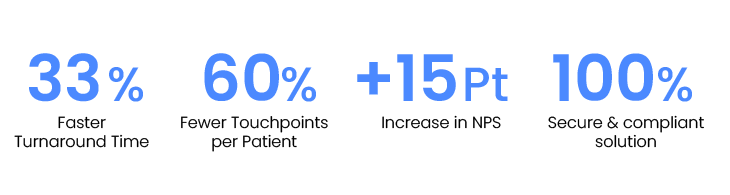
Healthcare providers can seize the opportunity of digital innovation to accelerate business and operational efficiencies so that they can enhance patient care and engagement throughout their lifecycle.
Learn how Lightico can accelerate your organization's patient experiences.
Experience the Interactive Video